Below are some basic Instructions for using the Osteogen Bone Block
Product Characteristics of Osteogen Malleable Bone Block (MBB)
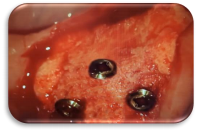
A Tenting Screw Kit is ideal for holding the soft tissue and resorbable membranes crestally or buccally to cover the Osteogen Malleable Bone Block The flat head surface with a curved edge provides ideal function without damaging the soft tissue. The appropriate screw length should be selected given the specific clinical case depending on the defect size. Three to four screws should be used to secure the MBB and hold the soft tissue, Figure 2 & 4. A resorbable membrane is required for all grafting procedures. MBB needs hydration with blood coagulum to become malleable and be compress into place.
Fig. 1: Harvesting Anterior Lower Cortex
Widening a narrow lower anterior ridge is typically challenging due to lack of vascularity in this case. The buccal plate may be fused crestally half way down and may need to be removed using a piezo handpiece. Harvesting this buccal cortex creates a thin plate that can be used in a surgical approach that is similar to Dr. Khoury’s autogenous bone block technique 1. Once cortex is removed, use a 2.5mm twist drill to make “bleeders” in order to trigger the Regional Acceleratory Phenomenon (RAP) 2.
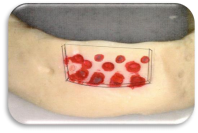
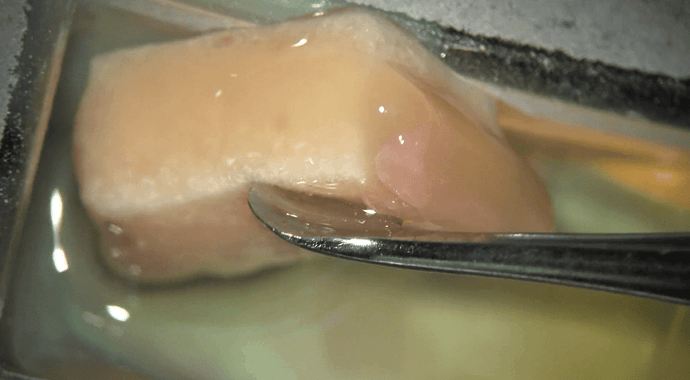
Fig. 2: Hydrating the MBB & Utilizing Harvested Buccal Cortex
Use medullary blood or PRF to hydrate the hydrophilic MBB. Aggressively compact the MBB and fill additional voids around the defect site. Make 2mm holes through the harvested plate and use tenting screws to secure the MBB between the plate and the host bone.
The use of autologous growth factors (e.g., PRF) will enhance the mechanical properties of the OsteoGen® MBB and may be useful during healing. If using PRF, a traditional “sticky bone” approach should be followed where the block is hydrated with plasma (containing cells) following a short 3-minute centrifugation and allowed to coagulate 3. A membrane is required to secure with 5mm TriStar® screws, if primary closure is not possible.
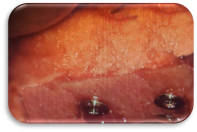
Fig. 3: Widening a Compromised Posterior Ridge
Using a minimum diameter of 2.5mm twist drill, make holes horizontally through the cortex. These “bleeders” will increase vascularity containing the bone-forming cells and procure medullary blood from the cancellous bone containing osteoclast/osteoblast cells in order to trigger the Regional Acceleratory Phenomenon (RAP)2. The osteoclast cells will remove and digest the OsteoGen® MBB, and the
osteoblast cells will establish new bone formation. Roughen the entire cortex area aggressively for MBB adaptation and stability.
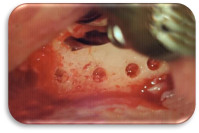
Fig. 4: Using a Resorbable Membrane
The MBB should be covered with a membrane to help restrict soft fibrous tissue invagination to assist in faster bone formation. Secure membrane using long screws. Attaining and maintaining a tension free tissue closure during surgery and healing phase is key to a predictable and successful outcome to control downward migration of ephilium 4-6.
References
- Khoury F and Hanser T. Mandibular bone block harvesting from the retromolar region: a 10-year prospective clinical study. Int J of Oral Maxillofac Implants 2015;30(3)688-697.
- Frost HM: The Regional Acceleratory Phenomenon: a Review. Henry Ford Hosp Med Journal 1983;31(1):3-9.
- Pinto NR, Temmerman A, Castro AB, Cortellini S, Teughels W, QuirynenM. Guidelines for the use of L PRF Flow Charts: Step by Step Approach Leucocytes and Platelet Rich Fibrin in Different Intra-oral Applications Applying the IntraSpin Concept. researchgate.net/publication/321873582
- Spivak JM, Ricci JL, Blumenthal NC, Alexander H. A new canine model to evaluate the biological response of intramedullary bone to implant materials and surfaces. J Biomed. Mater Research.1990; 24:1121-1149. 5. Ricci JL, Blumenthal NC, Spivak JM and Alexander H. Evaluation of a low-temperature calcium phosphate particulate implant material: Physical-chemical properties and in vivo bone response. J Oral Maxillofacial Surgery. 1992; 50: 969-978.
- Valen M and Ganz SD. Part I: A Synthetic Bioactive Resorbable Graft (SBRG) for predictable implant reconstruction. J Oral Implantology. 2002; 28(4): 167-177.